The Anatomy of the Neck, Part Four: The Muscles and the Meridian Positions
on November 15, 2014If you’ve a reasonable idea of where the muscles in the neck are, the meridians fall relatively easily into place.
However, if this is the blog post that you have been waiting for I am using points and cun (cun = the width of the client’s thumb at the base of the thumbnail) as well as muscles to assist you.
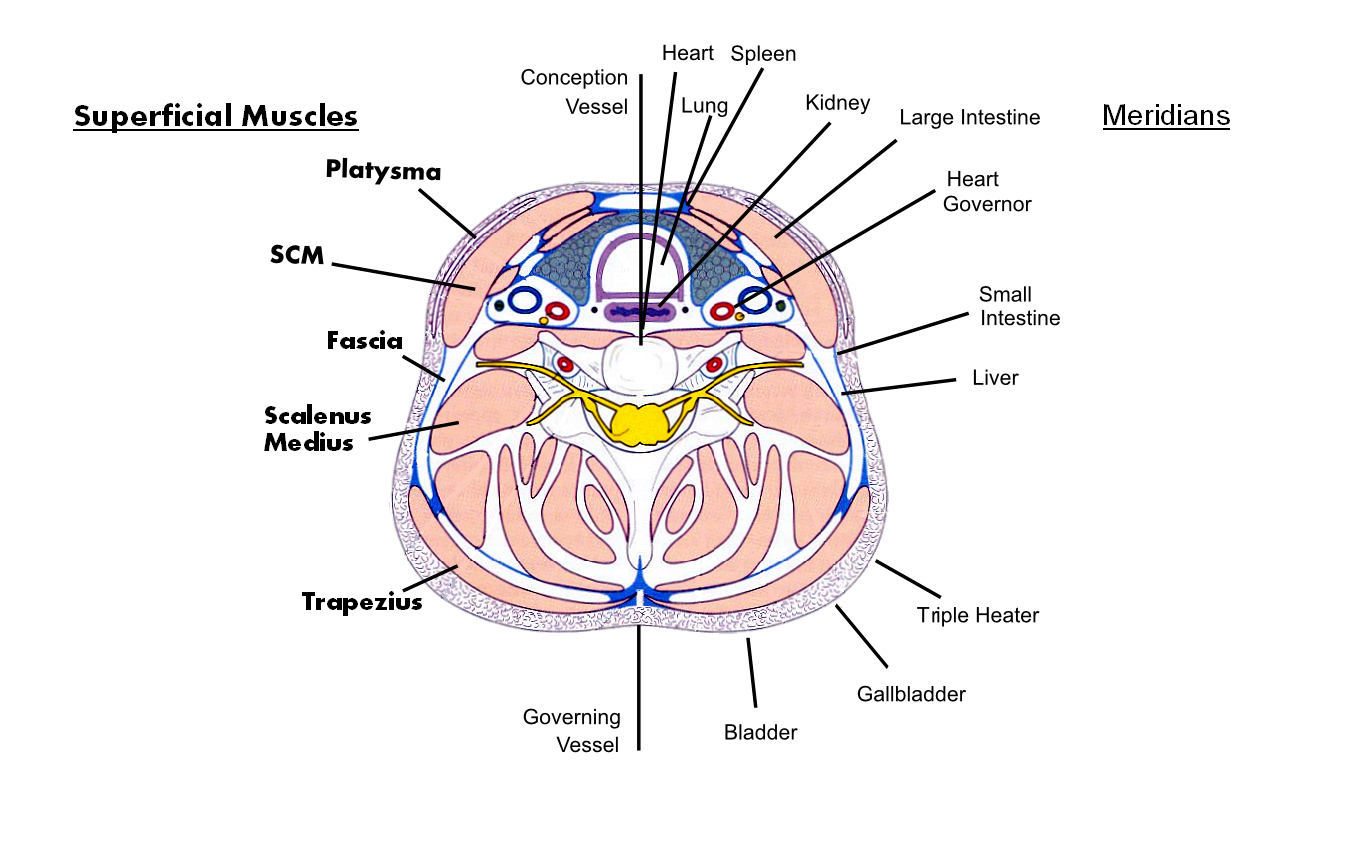 I have tried to show how the meridians relate to muscles and structures within the neck.
I have tried to show how the meridians relate to muscles and structures within the neck.
PLEASE NOTE: My choice of meridian position is at C6 and relates to MUSCLES.
Also, note that higher in the neck, Spleen and Small Intestine meridians cross over
The Meridians
Heart: 0.5 cun from CV, light yet deep and warm. Free flowing and open. Moves to the root of the tongue.
Heart Governor: Feel for the carotid pulse in the neck and angle your pressure towards the centre at approximately 45 degrees.
Kidney from Kid. 27: it runs upwards along the edge of the laryngeal cartilage and finishes here as it goes towards the thyroid gland.
Stomach: For me is 1.5 cun lateral to the larynx crossing the platysma muscle and sitting on the medial superior surface of the Sternocleidomastoid (herein referred to as the SCM) which is covered by the platysma.
Large Intestine, from L.I. 16: On the upper aspect of the shoulder, in the depression medial to the acromial process and the lateral extremity of the clavicle and scapular spine. Take a straight line until you meet the posterior edge of the SCM. This is L.I. 18 at the level of the top of the Adam’s Apple and on the belly of the muscle. It then flows directly to the corner of the Ali Nasi and under the nose, through the filtrum to the opposite side.
Spleen: Remember that the spleen is about quality. So follow the “flesh” across from Sp. 20 in the space between ribs 2 and 3 and 6 cun lateral to the base of the medial aspect of the S.C.M.. Now go slightly posterior to that place and feel the “interior quality” of the membrane as it climbs and meets St. 6.
Small Intestine: Find the lower border of C7 and 2 cun lateral is S.I. 15, located on the posterior edge of the SCM. Go upwards on the posterior edge of the SCM until you are parallel to L.I. 18, then cross the SCM, moving towards the posterior inferior angle of the mandible and the anterior border of the mandible (S.I.17).
Liver: I find that Liver can move a lot at its upper end from just underneath the mandible (perhaps connecting with a Heart meridian extension) to slightly behind the ear on the anterior superior edge of levator scapulae.
Gallbladder: Running up from GB 21 it sits on the anterior edge of the upper trapezius until it rises following the postero-lateral edge of the trapezius, to the hollow at the base of the skull between the origins of the SCM and lateral edge of the trapezius.
Triple Heater: Start from T.H.15 in the shoulder hole anterior to GB 21 and anterior to S.I. 13. This then flows upwards just behind the line of GB. Yet more on the fleshy edge of the trapezius. It exits the neck at T.H. 18 where the point is located in the depression on the mastoid bone in line with the rim of the ear.
Bladder: Rising from Bl. 11 at the lower edge of the spinous process of T1, 1.5cun from the midline. It flows superiorly to Bl.10 moving medially, slightly to a point on the edge of the trapezius muscle as it joins with the occiput. The channel then flows into the head ending at the inner canthus of the eye.
The meridian pathways described here are a mix of Zen meridians and acupuncture points and pathways. the pathways are always flexible in their position and for me they show the major energetic within them; whereas, acupuncture points are less mobile in their location.
You need to practice (Oh no! Not again!) and discover your preferred line of contact.
Neck Problems
Metabolic problems such as Ankylosing Spondylitis are NOT part of this blog. What I am writing about is “stuff” that we come across on a daily basis. Remember, if you use bodywork on a problem/symptom and it makes it worse, you need to find another form of treatment to “hands on” therapy.
Neck problems are always connected to some form of emotional disturbance or imbalance. Let’s take whiplash for example. First there is the violent physical movement, creating shock, this depending on the life of the client, will create any of the following.
Fear
Anger
Grief
Worry
Over thinking
Working through these via the neck muscles can be a slow process.
Sticking the head into some supportive collar, unless there is serious muscle damage, will only compound the problems that the client has to deal with. At this point as practitioners, we are definitely going against conventional practice and to overcome the doubt of the client in this process requires courage from us and the courage and trust of our client.
For everything from headaches, wry neck, muscle spasms, muscle weakness, trapezius strain and cervical root pressure can all come under 3 clear TCM headings.
1. Excess (heat, swelling etc.)
2. Deficiency (swelling with cold, pain on movement)
3. Stagnation (this often relates to the clients fear movement and unresolved shock, anger, worry etc.)
If you think in these terms, ask yourself and the client the WHAT, WHERE, WHEN, WHY ,WHO and HOW questions.
You will then understand:-
The principle emotion
The presenting symptom
Whether and on what level you are dealing with excess, deficiency and stagnation.
Remember also that here will always be a mix of excess, deficiency and stagnation and all of the emotions.
Palpating and finding the exact places of pain, excess or lack of movement tells you the muscles and ,meridians you have to work. It is imperative that you forget initially the background of the symptom. The PAYING client wants relief and quickly. So focus your treatment on releasing and reducing the pain and while you do this assess and talk with your client about continuing visits. Rarely does one session solve the problem.
For an injury such as whiplash, warmth and gentle fascial movement are the first order of the day. Depending on how soon after the injury you see them, you may be dealing with the immediate shock, pain, anger, grief, etc.. If you see them many days or weeks after the incident, has it moved to a deep seated situation where painful obstruction syndrome is what you are dealing with?
Painful Obstruction Syndrome is that state where the body has held an “injury” without it healing for a long time. Perhaps the same injury has been repeated. The damaged tissue does not repair, but goes into a state of suspended animation re emerging when a stress factor wakes it up and the pain returns. This is a deep seated and often mid to long term recovery process.
We are “hands on” body workers, we need to accept our limitations, be honest, sometimes painfully so with our clients and our prognosis for their recovery. Remember also you may only see them for one hour a week or even less, they need to accept responsibility for themselves and their healing for some of the period during the other 167 hours of that week.
NEXT
The video……
